Leukemia and the Immune System
- sunshine4cancerkid
- Aug 13, 2024
- 12 min read
Updated: Oct 11, 2024
By: Zaara Hossain, Sumeet Seal, Neha Shiju, Maliha Akbar, and Shan Nizam
Discussion
Leukemia is the most common form of cancer in children and receiving a diagnosis can completely change the quality of life of a child. Leukemia accounts for nearly 30% of all childhood cancers. Understanding its impact not only contributes to the scientific community’s knowledge, but it also aids in improving treatment regimens and patient outcomes. Exploring the effects of leukemia on the immune system can provide insights into how the disease alters immune functionality both before and after treatment, which is necessary for developing targeted therapies and supportive care strategies. For this reason, we have chosen to research this disease and thoroughly outline the changes the immune system undergoes in a patient that has leukemia. Throughout this paper, we will primarily discuss two types of leukemia that affect children: acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML). The purpose of this paper is to answer the question: How does the progression of leukemia affect the functionality of the immune system prior to treatment and post-treatment?
Abstract
Leukemia is particularly devastating in kids since it is the most common type of cancer in children and adolescents, 25.1%, and ranks as the second leading cause of cancer deaths in the US among children under 20, at a high level of 22.7%. The development of leukemia has a significant impact on immune system functionality during both pre-treatment and post-treatment periods. Leukemia is a type of blood cancer that originates in the bone marrow. It causes an uncontrolled production of abnormal WBCs (White blood cells). These WBCs are termed leukemic cells, and their action interferes with the proper functioning of a patient's immune system, making them more prone to infections. Different modes of treatment, most notably in the form of radiation therapy, chemotherapy, and stem cell transplantation, are designed to kill the leukemic cells and restore normal hematopoiesis. During pre-treatment of leukemia, the children sometimes need a blood/platelet transfusion due to the leukemic cells stopping the bone marrow from producing normal blood cells, as well as fluids in their bloodstream (IV) and medicine to protect their kidneys from the chemical reaction involving the breakdown of the leukemia cells. Additionally, antibiotics might be needed in a severe case since the patient will not have enough normal white blood cells fighting against infections. In post-treatment cases of leukemia, the patient goes through an immune recovery phase dependent on the type of treatment and the patient's condition.
Introduction
Leukemia is a specific type of cancer that affects the blood. It causes rapid growth of dangerous blood cells in the bone marrow. It generally affects adults over 55 and children below 15 ("Leukemia—Patient Version"). There are various types of leukemia. The type of leukemia depends on the blood cell that becomes cancerous and the rate at which it grows throughout the body ("Leukemia—Patient Version"). Leukemia presents itself in various forms. For instance, there is acute lymphoblastic leukemia, chronic myeloid leukemia, and many more. To categorize these types, there are mainly four types that are referred to (Stanford Medicine). The types include acute lymphoblastic leukemia, acute myeloid leukemia, chronic myeloid leukemia, and chronic lymphocytic leukemia (Stanford Medicine). Acute myeloid leukemia is the most fatal of them all. The five-year survival rate for AML is 29.5 % (Cunha).
The immune system has an important role in defending against malignancies, such as leukemia. In children diagnosed with leukemia, particularly acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML), there are significant changes in immune function due to both the disease itself and its treatment modalities. These changes to the immune system will be studied throughout this paper.
Diagnosis
When diagnosing leukemia there are several symptoms and circumstances to consider. To diagnose leukemia, doctors typically start with a physical exam and a Complete Blood Count (CBC) or a flow cytometry. A flow cytometry is a laser beam used to identify leukemic cells in a blood sample. This sensitive technology allows for the differentiation of myeloblastic and lymphoid. If a person has an abnormal count of white blood cells or a particularly low count of red blood cells, and platelets, this is also an indicator for leukemia. Exact causes and indicators are unknown, however, risk factors include family history (genetics), chemotherapy, or repeated exposure to certain chemicals. For example, benzene, which is commonly found in industrial processes, synthetic fibers, lubricants dyes, and cleaning products. Symptoms can vary from different people, however, common symptoms in children include pale skin, feeling tired, weak or cold, dizziness, headaches, shortness of breath, long-term or frequent infections, tenderness, and bone pain.
Medical Professions
Accurately diagnosing and treating a case of leukemia will require a multidisciplinary team of medical professionals whose diverse skills and rigorous educational backgrounds merge into close collaboration to ensure comprehensive, and thorough care. Hematologists study blood disorders, diagnose leukemia through blood tests and bone marrow biopsies, and manage treatment plans at a median salary of $303,501. Their education includes a medical degree followed by an internal medicine residency, 3 years, and a fellowship in hematology, 2-3 years. Radiologists, with a median annual salary of $449,390, use imaging techniques including X-rays, CT scans, MRIs, and PET scans to detect abnormalities and guide procedures such as bone marrow biopsies. They have undergone extensive training for their specialty, including a 4-year residency in radiology and for many, additional fellowship training in a subspecialty. Oncologists, whose average salary is around $331,051 annually, are responsible for diagnosing leukemia, outlining the proper treatment plans that involve chemotherapy and radiation, and integrating care across specialties. Their educational track includes an internal medicine residency for 3 years and a fellowship in oncology or hematology-oncology for 2-3 years. Pathologists, with a median salary of $300,600, are critical to diagnosing leukemia by examining the blood sample, bone marrow biopsies, and other tissues through a microscope that will inform treatment decisions by hematologists and oncologists. They complete a 4-year residency in pathology, then often specialize with additional fellowship training. General surgeons also perform highly relevant surgical interventions, such as implanting ports for chemotherapy administration in cooperation with radiologists and pathologists; their median salary is about $426,900. Their educational background includes a long residency in general surgery of 5-7 years and, for some, even additional sub-specialization. General practitioners, whose median salaries are around $222,590, may often be the first to identify symptoms of leukemia, sending their patients to consultants and continuing care and follow-up for these patients. They also do a residency in family medicine, internal medicine, or pediatrics; this takes 3 years. Oncology nurses are very essential in the delivery of treatments and management of side effects, and they are crucial for emotional support while performing their duties with a median salary of $83,100. Most of them acquire a Bachelor of Science in Nursing and then pursue advanced certifications or degrees. The teamwork of these professions is essential, with hematologists collaborating with pathologists for accurate diagnosis, radiologists and oncologists working together to monitor and adjust treatment plans, and oncology nurses coordinating care across the entire team. General surgeons and GPs support treatment through surgical procedures and ongoing patient management, ensuring seamless and comprehensive care. This approach involves not only these key specialists but also dietitians, social workers, and pharmacists, who all work together to address every aspect of a leukemia patient’s needs, from diagnosis to treatment and beyond.
Treatments
When discussing the treatment regarding children who have leukemia, it is crucial to mention the different subtypes of leukemia that affect children: ALL (Acute Lymphocytic Leukemia), AML (Acute Myeloid Leukemia), APL (Acute Promyelocytic Leukemia), JMML (Juvenile Myelomonocytic Leukemia), and CML (Chronic Myeloid Leukemia). Many of these different sub-groups of leukemia use chemotherapy, chemo-based drugs, and other specific drugs (ATRA, daunomycin, cytarabine, etc.) as the primary treatment. Additionally, it’s important to note that secondary treatment options such as stem cell surgeries, and newer drugs (enasidenib, olutasidenib, and ivosidenib) are great options if the primary treatment methods don’t seem to work or if leukemia persists. Moreover, if the leukemia relapses, the patient will undergo stem-cell transplants, and in extreme cases, the patient will participate in clinical trials. However, some of these subtypes of blood cancer known as JMML and CML have no clear treatment option (no cure) yet but research is underway to hopefully cure the children in the future who suffer from these subtypes. The treatment for many of these different leukemia subtypes occurs in three stages: Induction, Consolidation, and Maintenance. The purpose of the induction phase is to destroy as many cancer cells as possible to achieve remission. The next phase, consolidation, kills any remaining cancer cells. Lastly, the maintenance phase aims to prevent the relapse of cancer after induction and consolidation therapy.
Statistics
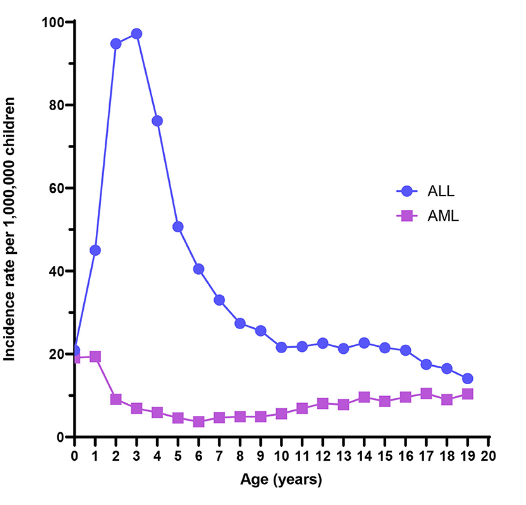
Figure 1. Acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML) incidence rates from the US Surveillance, Epidemiology, and End Results program, 2000–2017.
The above graph showcases the prevalence of acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML) per 1 million children. As can be seen in the graph, the rate of diagnosis of ALL and AML depends on the age of the child. In ALL, age 4 has the highest rate of diagnosis (with 100 children per 1 million). Whereas in AML, age 1 has the highest rate of diagnosis (with 20 children per 1 million). The AML line is also more evenly spread and comparatively more stagnant whereas the ALL line has more variation.
Figure 2. Childhood Cancer Rates Pie Chart (American Childhood Cancer Organisation).
The second figure (shown above) depicts the rates of different cancers in children. The pie chart conveys that leukemia is the most common, with CNS (central nervous system)/brain cancer being the second most common, lymphomas being the third most common, and many others being significant but affecting less than (or equal to) 10% of children. It is important to understand from this graph that leukemia is extremely prevalent in children since it affects 23% of children. This is not a negligible rate and therefore must be addressed on a global scale.
Figure 3. U.S. Prevalence of Blood Cancer in Children below 15 years (Leukemia and Lymphoma Society 5).
This figure depicts the prevalence of blood cancer in children below 15 years. It specifically only focuses on the U.S. making it invalid on a global scale, however, it provides insight into the country’s cases of blood cancer. The table shows that 26,880 children below 15 have leukemia. This is notably higher than any of the other blood cancers on the table.
Figure 4. Five Year Survival Rates based on Year of Diagnosis (Leukemia and Lymphoma Society 3).
The last figure depicts the five-year survival rates for different blood cancers based on the year of diagnosis. The figure shows that the survival rates have increased in recent years for most blood cancers although myelo-dysplastic syndromes (MDS) is the exception here. Leukemia has shown an increase in survival rate with time, with it being at 69% between 2012-2018.
Impacts
Leukemia leads to the rapid increase of abnormal blood cells, reducing the amount of healthy white blood cells. This impacts children with leukemia such that they often struggle to fight off infections and are more likely to fall ill with fevers. They are likely to experience dizziness and nausea, along with other symptoms. Leukemia affects children’s everyday lifestyles because they are likely to display pale skin and are prone to unexplained bruising or bleeding. These symptoms can significantly impact a child’s daily activities and overall quality of life. For example, due to the possibility of frequent bruising, a child with leukemia may be restricted from playing at the playground or with other children due to the risk of getting injured. They are also more prone to fatigue, growth delays, hearing loss, and the risk of relapsing once they receive treatment (such as chemotherapy). Chemotherapy is the primary form of treatment and although it can be effective, it weakens the immune system and can lead to anemia. This can lead to prolonged hospitalization following treatment for certain children. Another concern about treatment is that children can develop infertility in the future. These factors impact the youth because there are a lot of risks that require precaution before and after treatment. The survival rate of leukemia has increased over the years so children are more likely to live with treatment following the initial diagnosis. However, survivors are at risk for late effects such as secondary cancers (due to radiation therapy), cardiovascular issues, and endocrine problems (like thyroid dysfunction). This leads to a need for follow-up care as a child reaches adolescence and adulthood.
Along with physical impacts, psychological factors need to be taken into consideration. Receiving a diagnosis for cancer is life-changing, particularly for young children who can’t fully understand what the diagnosis means for them. Children may experience anxiety, fear of medical procedures, or experience stress while thinking about their future. This stress can manifest as depression or behavioral issues. Leukemia is disruptful of a child’s everyday life and a child with leukemia may feel isolated from peers. Due to frequent hospital visits or compromised immune systems that require them to avoid crowds (especially during treatment), children may miss out on social activities like school events or playdates. Unfortunately, children may face stigma from peers who do not understand their condition or who are afraid of contagion due to the child’s weakened immune system. Frequent absences from school can also negatively impact academic progress and create gaps in learning. The diagnosis often affects not just the child but also family members such as parents and siblings. Parents may experience stress from managing treatment schedules and financial burdens due to healthcare costs. Overall, leukemia impacts the youth significantly due to physical and psychological changes that occur following a diagnosis. As time goes by and the scientific community learns more about leukemia, the prognosis has significantly improved. With advances in treatment, children with the disease have up to a 90% survival rate, with many going on to live happy, productive lives (Yale Medicine).
Conclusion
Pediatric leukemia remains one of the most crucial challenges in childhood health today because of its significant impact on young patients and their families. The various forms of this disease (primarily ALL and AML) require rigorous treatment regimens and supportive care. The prognosis for pediatric leukemia has improved over the past few decades due to advances in medical science, however, disparities still exist based on access to healthcare services, and geographic location. By raising public awareness of leukemia, more people will be equipped with knowledge about the symptoms and risks of leukemia. Parents may be able to notice symptoms quicker than those who are unaware of what leukemia is. This can increase the chance of early intervention and improve outcomes. Scientists are working on improving outcomes for children diagnosed with leukemia through innovative therapies and supportive care systems. It is our responsibility to work on creating an environment of understanding within our communities about its prevalence and impact on young lives. As students, we can develop educational campaigns to explain leukemia and distribute flyers in schools, hospitals, and community centers. We can engage the public through social media platforms and discuss leukemia through infographics and podcasts featuring survivors. Community events such as walks for leukemia and fundraisers can unite the community and lead to more support for those with leukemia. As we work together to improve awareness about leukemia, we are strengthening our community and advocating for children who need our support.
Bibliography
Acco. Cancer in Children,
1 July 2015, www.acco.org/blog/cancer-in-children/.
American Childhood Cancer Organisation. "Cancer in Children." American Childhood Cancer Organisation,
1 July 2015, www.acco.org/blog/cancer-in-children/. Accessed 12 Aug. 2024.
“Benzene.” Wisconsin Department of Health Services,
“Blood Cancer Medical Team: Hematologist, Oncologist, and More.” WebMD,
WebMD, www.webmd.com/cancer/lymphoma/your-medical-team. Accessed 13 Aug. 2024.
“Chemotherapy.”
Https://Www.Lls.Org/Leukemia/Acute-Lymphoblastic-Leukemia/Treatment/Chemotherapy,www.lls.org/leukemia/acute-lymphoblastic-leukemia/treatment/chemotherapy. Accessed 13 Aug. 2024.
“Childhood and Adolescent Blood Cancer Facts and Statistics.” Childhood and Adolescent Blood Cancers,
www.lls.org/facts-and-statistics/childhood-and-adolescent-blood-cancer-facts-and-statistics#:~:text=The%20most%20common%20types%20of,thyroid%20cancer%20(6.2%20percent). Accessed 13 Aug. 2024.
“Childhood Acute Myeloid Leukemia Treatment.” Childhood Acute Myeloid Leukemia
Treatment www.cancer.gov/types/leukemia/patient/child-aml-treatment-pdq. Accessed 13 Aug. 2024.
Cunha, John P. "Which Type of Leukemia Is Most Fatal?" E Medicine Health,
www.emedicinehealth.com/which_type_of_leukemia_is_most_fatal/article_em.htm. Accessed 12 Aug. 2024.
“Diagnosing Leukemia.” Yale Medicine, Yale Medicine, 11 Aug. 2022,
“Induction Treatment for Childhood Acute Lymphoblastic Leukaemia (All).” Cancer Research UK, Cancer Research UK, 2
“Leukemia.” Hematology.Org,
www.hematology.org/education/patients/blood-cancers/leukemia#:~:text=Your%20doctor%20will%20conduct%20a,counts%20can%20also%20indicate%20leukemia. Accessed 13 Aug. 2024.
“Leukemia.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 21 Sept. 2022,
Leukemia and Lymphoma Society. "Updated Data On Blood Cancers." PDF.
Leukemia—Patient Version." National Cancer Institute, www.cancer.gov/types/leukemia. Accessed 12 Aug. 2024.
“Leukemia in Children.” Yale Medicine, Yale Medicine,
24 Sept. 2022, www.yalemedicine.org/conditions/leukemia-in-children. ‘
Marcotte, Erin L., et al. “The Prenatal Origin of Childhood Leukemia: Potential Applications for Epidemiology and Newborn Screening.” Frontiers, Frontiers,
“Pediatric Leukemias.” Children’s Hospital of Philadelphia, The Children’s Hospital of Philadelphia,
11 Sept. 2014, www.chop.edu/conditions-diseases/pediatric-leukemias.
Professional, Cleveland Clinic medical. “Leukemia: Symptoms, Signs, Causes, Types & Treatment.
Cleveland Clinic, 18 May 2022, my.clevelandclinic.org/health/diseases/4365-leukemia.
“Relapsed/Refractory Acute Lymphoblastic Leukemia (ALL).” Children’s Hospital of Philadelphia, The Children’s Hospital of Philadelphia,
“Treatment of Children with Acute Lymphocytic Leukemia (ALL).” American Cancer Society,
www.cancer.org/cancer/types/leukemia-in-children/treating/children-with-all.html. Accessed 13 Aug. 2024.
“Treatment of Children with Acute Myeloid Leukemia (AML).” American Cancer Society,
www.cancer.org/cancer/types/leukemia-in-children/treating/children-with-aml.html. Accessed 13 Aug. 2024.
“Treatment of Children with Acute Promyelocytic Leukemia (APL).” American Cancer Society,
www.cancer.org/cancer/types/leukemia-in-children/treating/children-with-apl.html. Accessed 13 Aug. 2024.
“Treatment of Children with Chronic Myeloid Leukemia (CML).” American Cancer Society, ACS,
www.cancer.org/cancer/types/leukemia-in-children/treating/children-with-cml.html. Accessed 13 Aug. 2024.
“Treatment of Children with Juvenile Myelomonocytic Leukemia (JMML).” American Cancer Society,
www.cancer.org/cancer/types/leukemia-in-children/treating/children-with-jmml.html. Accessed 13 Aug. 2024.
“Treatment Roles - Cancer Treatment.” Siteman Cancer Center, 8 Sept. 2020,
“Unlock the Power of Pay.” Salary.Com,
www.salary.com/. Accessed 13 Aug. 2024.
"What Are the Different Types of Leukemia?" Stanford Medicine,
stanfordhealthcare.org/medical-conditions/cancer/leukemia/types.html. Accessed 12 Aug. 2024.
“What’s New in Acute Myeloid Leukemia (AML) Research?” American Cancer Society,
www.cancer.org/cancer/types/acute-myeloid-leukemia/about/new-research.html#:~:text=IDH%20inhibitors%20can%20help%20leukemia,now%20being%20studied%20as%20well. Accessed 13 Aug. 2024.
“Who’s Who on Your Healthcare Team.”
Https://Www.Lls.Org/Treatment/Communicating-Your-Specialist/Whos-Who-Your-Healthcare-Team, www.lls.org/treatment/communicating-your-specialist/whos-who-your-healthcare-team. Accessed 13 Aug. 2024.
“Your Care Team.” Leukaemia Foundation,






Comments