Astrocytoma: From Diagnosis to Management – A Comprehensive Overview
- sunshine4cancerkid
- Aug 13, 2024
- 27 min read
Updated: Oct 12, 2024
Adil Mukhi, Nimeesha Komatireddy, Srikarthi Jaggavarapu, Ariana Pham, Najatu Shaibu, Saanjh
Words: 66595
Adil Mukhi | Writer/Researcher | Glenforest Secondary School & International Baccalaureate
Nimeesha Komatireddy | Writer/Researcher | Arnold O. Beckman High School
Srikarthi Jaggavarapu | Writer/Researcher | Smithtown High School East
Ariana Pham | Writer/Researcher | Simon Fraser University
Najatu Shaibu | Writer/Researcher | Fijai Senior High School.
Saanjh | Writer/ResearcherAFFILIATION
Table Of Contents
Abstract
Astrocytomas are a prevalent type of glioma originating from astrocytes, a type of glial cell in the brain. They constitute a significant portion of brain tumors in both children and adults. Recent research has enhanced our understanding of astrocytomas by exploring the tumor microenvironment and genetic mutations, such as IDH1 and IDH2, which influence growth, progression, and treatment resistance. These tumors present a major challenge due to their infiltrative nature and resistance to conventional therapies, highlighting the need for innovative treatments.
Astrocytomas are confined to the central nervous system (CNS) and do not spread to other organs. They multiply within the brain by infiltrating surrounding tissue, making them difficult to remove surgically. The rapid growth is driven by genetic mutations and interactions with the brain's microenvironment.
Symptoms vary by age: in children, astrocytomas often affect the cerebellum or brainstem, causing balance and coordination issues, headaches, nausea, and developmental delays. In adults, they are more common in the cerebral hemispheres, leading to headaches, seizures, personality changes, cognitive difficulties, and motor weakness, depending on the tumor’s location.
Astrocytomas are classified into different grades based on their aggressiveness and malignancy, ranging from low-grade (slow-growing) to high-grade (fast-growing). Lower-grade astrocytomas, such as Grade I and II, often have a better prognosis but can progress to more aggressive forms over time. High-grade astrocytomas, such as Grade III (anaplastic astrocytomas) and Grade IV (glioblastomas), are more aggressive and challenging to treat due to their rapid growth and tendency to invade surrounding brain tissue. Effective management of astrocytomas involves a combination of surgery, radiation, and chemotherapy, with ongoing research focusing on developing targeted therapies and personalized treatment strategies to improve patient outcomes.
Introduction
Brain and Spinal Cord Tumors
A tumor is a mass of abnormal cells that either form into new growth or the growth was there when you were born - known as congenital tumors. Tumors occur when the genes that regulate cell growth are not functioning properly or something goes wrong in their function, which causes cells to grow and divide out of control. Tumors can form anywhere in the body. Brain and Spinal Cord tumors occur in the brain and spinal cord tissue, which comprise the Central Nervous System (CNS).
Tumors are either benign or malignant. Benign tumors can be slow or fast-growing, do not evade other parts of the body, and most of the time these tumors can be removed from surgical procedures. Malignant tumors are usually fast-growing, some can be surgically removed but some have undefinable edges that are hard to remove surgically. In tumors that occur in the CNS, there are primary and secondary tumors also known as Metastatic tumors. Primary tumors are growths in the brain and spinal cord and can be both malignant and benign. Secondary tumors (Metastatic) of the CNS are caused by cancer cells that break away from the primary tumor and come to the CNS. There are many types of brain and spinal cord tumors such as Gliomas, a group of tumors that start with glial cells in the brain, Embryonal tumor, for example, Medulloblastomas, which is the most common embryonic tumor, Chordomas, Neuroblastomas, etc (Pichaivel et al.). Symptoms used to diagnose a tumor in the central nervous system are mostly based on the size and location of the tumor. The most common symptoms of a tumor are persistent headaches, nausea and vomiting, a feeling of pressure inside the skull, problems of hearing and vision, motor issues, pain in specific areas of the spine or pain radiating off of the spine to other locations, balance issues, and numbness and sensory changes. Neurological exams; diagnostic imaging, such as MRI; and laboratory work are common ways to diagnose brain and spinal cord tumors. Treatments include radiation therapy, surgery, chemotherapy and targeted therapy (National Institute of Neurological Disorder and Stroke).
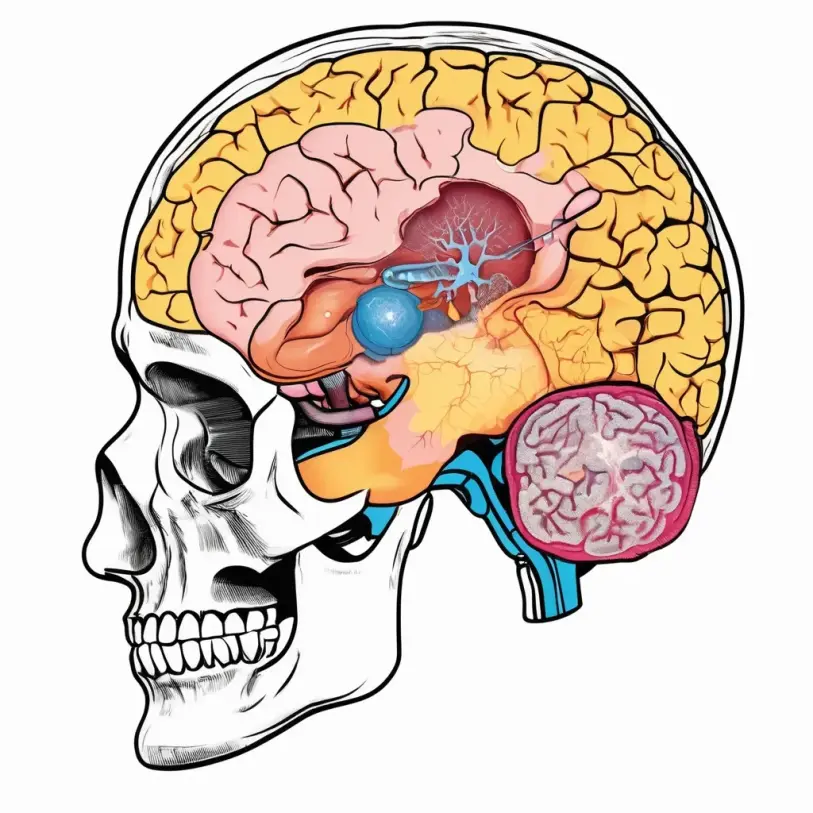
Astrocytoma
Astrocytoma is a type of brain and spinal cord tumor part of Gliomas. Gliomas begin from glial cells, and in the case of Astrocytoma, the tumor grows from cells in the glial subgroup Astrocytes, which are star-shaped glial cells. These star-shaped glial cells play an essential supporting role in functions of the central nervous system including brain-blood barrier development and maintenance, stimulating immunological responses, etc. Astrocytomas are genetically obtained, and there has been a linkage between hereditary syndromes like Cowden and Neurofibromatosis Type 1 to the increased rates of Astrocytoma development. There are also genetic mutations that could occur and lead to the development of Astrocytoma. Similar to most brain tumors, Astrocytoma is presented with symptoms like weakness, numbness, seizures, and aphasia. While, generalized symptoms due to edema and increased intracranial pressure can cause headaches, vision deficits, and emesis. Astrocytomas are mostly treated by radiation, chemotherapy, and surgical resection of the tumor. These treatments take a part in the medical management of both low and high-level Astrocytomas to do things like reduce symptoms, improve prognosis, and prevent the tumor from becoming malignant (Willman et al.). Pilocytic Astrocytoma is the most common pediatric brain tumor for children 5-14 years old. Pilocytic Astrocytoma (PA) are most usually found in the base of the brain (cerebellum), but can also occur in all parts of the brain. PAs are generally slow-growing and can spontaneously regress based on time (Bornhorst, et al.). This research will predominantly contain comparisons between Astrocytomas in adults in relation to children, including how Astrocytomas grow quickly but tend to not affect other body parts.
Discussion
Why Astrocytoma?
The recent scientific discovery shows that the microenvironment of this tumor growth and specific genetic mutations play in tumor progression and resistance. Glioblastomas have been discovered to harbour complex interactions with surrounding neural and immune cells which can significantly influence the tumor’s behaviour and response to treatment (Pratibha et.al). Studying astrocytomas will enable the understanding of the brain’s functioning and the role of Glial cells which are not well explored like neurons.
Novel molecular markers and pathways such as IDH1 and IDH2 genes are common in lower-grade astrocytomas and are associated with better prognosis( Rohit Sharma). This has opened new ideas for targeted therapies.
Astrocytomas are a very common type of brain tumor in children and young tumors. (Karaba B et.al) Glioblastomas are very aggressive and poor rate of survival. Understanding these tumors can lead to better treatments and solutions.
Astrocytomas are difficult to treat because of their location in the brain, have the tendency to infiltrate surrounding brain tissue and are resistant to traditional therapies like Chemotherapy and Radiation (Gunnarsson T. et. al.). This triggers our research to find more effective treatment.
Researching Astrocytomas enables us to explore immunology as other fields have proved futile in addressing the disease.
How to Diagnose Patients
Signs and Symptoms Of Astrocytomas.
Astrocytoma, like all brain tumors, is an abnormal growth of cells within the brain, just that they originate from the glial cells. They can be mistaken for other neurological conditions like Meningioma, Multiple Sclerosis, Stroke, and Brain Abscess due to overlapping symptoms. Some of the symptoms are;
Headache and Seizures: A prominent symptom is periodic headaches which are severe in the morning or when lying down due to increased intracranial pressure. Seizure sessions are also associated with low-grade astrocytomas (Carstam et.al).
Imbalance and Coordination Issues: Victims tend to find difficulty with balancing their body in terms of walking, standing or any motor-related activities due to the growth of the tumor which tends to suppress certain brain locations associated with motor control. Also, the growth of the tumor disrupts certain neurological pathways and this is expressed in their coordination. (Kenneth et.al).
Speech Difficulties: Astrocytomas patients often have trouble speaking, understanding languages and forming words (Aldape et.al).
Weakness: Patients also experience weakness in their body, often on only one side.
Nausea and Vomiting: Due to increased pressure within the skull, victims experience vomiting and nauseous feelings.
Cognitive or Behavioural Changes: Patients often have memory loss and difficulty concentrating or solving problems (Ingela et.al).
Medical Equipment Used For Diagnosing Astrocytomas.
Many instruments are involved in the imaging and clinical studies of Astrocytomas. These include:
Magnetic Resonance Imaging: This is the primary tool employed in obtaining images used to determine the presence of astrocytomas.
MRIs can be used to identify the tumor’s growth, location and size (Djamil et.al).
Conventional MRIs: provide high-resolution images of the brain structure that could spot any new growth or development close to a tumor.
Contrast-Enhanced MRIs: involve the injection of a contrast agent to highlight the tumor and differentiate it from other surrounding tissues. Examples of the contrasting agents are Gadolinium.
Perfusion MRIs are used to measure blood flow in the brain and tumor. This enables evaluation of the tumor’s aggressiveness and intensity.
Diffusion-weighted MRIs help to diagnose MRIs by assessing the tumor’s cellular density, thus being able to distinguish between the grades of the tumor.
Magnetic Resonance Spectroscopy is an advanced MRI technique that measures the chemical composition of brain tissue. It helps to distinguish tumor types and grades by analyzing metabolites in the tumor area such as Choline, Creatine and N-acetyl aspartate.
2. Computer Tomography Scanner
This type of imaging device is used in the absence of MRIs. CT scans provide an introspect of the brain and help to detect tumors, swelling and bleeding. Conventional CTs provide cross-sectional images of the brain. CTs with Contrast use the injection of a contrast agent to enhance the visibility of the tumor.
3. Positron Emission Tomography Scanner
PET scans are instruments used to assess the metabolic activity of a tumor. In Astrocytomas, a PET can be used to identify a high metabolic activity which enables to infer high tumor grade or aggressiveness. They are often used in combination with CTs and MRIs to provide both anatomical and metabolic information (Clarke et.al).
Biopsy.
A Biopsy is a conclusive method to diagnose astrocytomas and determine their grade. This primarily involves sampling tissues from the tumor and analyzing it histologically. Stereotactic Biopsy is a minimally invasive procedure where a needle is guided by imaging to collect a tissue sample from the tumor. Surgical Biopsy is performed during tumor resection surgery to obtain a large sample or remove the tumor completely (Mayank et.al).
Electroencephalography.
Electroencephalography(EEG) is used to monitor electrical activity in the brain and can help diagnose seizures, a common indication of astrocytomas. It involves placing electrodes on the scalp to record the brain’s electrical signals. Abnormal patterns may then predict a tumor such as Astrocytoma that could be affecting the brain’s function (Clarke et.al).
Angiography
This method is used to visualize the blood vessels that supply blood to the tumor. Conventional Cerebral Angiography involves an invasive procedure where contrast dye is injected into the arteries and X-rays are taken to map blood vessels. Magnetic Resonance Angiography is a non-invasive MRI technique that is used to visualize blood vessels (Koak et.al).
Intraoperative Monitoring Equipment
This instrument is used during Astrocytomas surgery procedure to guide the surgeon and ensure maximal tumor resection while preserving critical brain functions (Carraba et.al).
Neurophysiological Testing
This is not an imaging technique, yet, they are used to evaluate cognitive function which is often affected by Astrocytomas. It helps to assess the impact of the tumor on memory, language and other cognitive abilities.
Medical Professions
Astrocytoma is a tumor that belongs to gliomas which has many treatments. Professionals such as neurosurgeons, neurologists, neuroradiologists, neuro-oncologists, radiation oncologists, and other specialists work together to provide the best remedy for patients (Weill Cornell Medicine Neurological Surgery).
Neurosurgeons
Neurosurgeons aim to lower the growth of tumors and obtain the tissue to further diagnose the tissue to establish an enhanced treatment plan (Mendoza, et al.). Neurosurgeon's career path includes enrolling in a four-year pre-medical education at a university/college. Afterwards, four years of medical school is required to obtain an M.D. or D.O. degree. Then, a one-year internship in general surgery is completed. Finally, neurosurgeons have to complete a residency to specialize in a certain area. Once this is completed, a surgeon/doctor can start doing their job in hospitals. This is the pathway for most doctors and surgeons (University of Rochester Medical Center). Neurosurgeons’ salaries can vary widely, ranging from $442,135 to over $875,000 annually. Factors such as location and type of practice play a role in the amount of pay one can get (Nabity).
Neurologists and Neuro-oncologist
Neurologists have the role of helping diagnose patients and recommending further steps to take when it comes to identifying the tumor. The neurologist and neuro-oncologist can recommend a specific type of treatment such as PET scans or MRIs when it comes to brain tumors and cancers. The average international pay for neurologists would be $347,715 (ZipRecruiter) while neuro-oncologists make an average of $352,527 per year (ZipRecruiter).
Radiation Oncologists
Furthermore, radiation oncologists help to lower the amount of tumor by performing External Beam Radiation Therapy, Stereotactic Radiosurgery, and Proton therapy. During external beam radiation, a linear accelerator rotates around the brain and sends high-radiation beams to a certain area in the brain (NYU Langone’s Perlmutter Cancer Center). The pay of these oncologists ranges from $169,000 to $530,000 according to data collected in 2024 (Nabity).
Overall, doctors and surgeons specializing in neurology and oncology tend to be the best doctors to receive treatment for any possible diagnosis of astrocytoma.
Treatments
Introduction to Astrocytomas
Overview of Astrocytomas
Tumors called astrocytes are derived from astrocytes, which are star-shaped glial cells found in the central nervous system (CNS). Depending on how malignant they are, they are categorized into low-grade and high-grade tumors. Glioblastoma (GB) is the most aggressive form of the disease, with a dismal prognosis and aggressive behaviour (Willman et al.). Usually, a multimodal strategy including radiation therapy, chemotherapy, and surgery is used to treat astrocytomas (Kabel et al.).
Importance of Understanding Treatment Options
A thorough awareness of the various treatment options is necessary for the effective management of astrocytomas. The grade, location, and genetic makeup of the tumor determine the specific treatment plan. Patients with astrocytomas now have better outcomes thanks to advancements in treatment approaches and the creation of targeted therapies. It is essential to comprehend these choices to maximize patient care and raise survival rates (Kessler et al.).
The Importance of Early Detection
Challenges in Early Detection
Because astrocytomas are frequently asymptomatic in their early stages, early detection is crucial for improving treatment outcomes, but it is still difficult. MRIs and other diagnostic imaging methods are vital for recognizing and describing these tumors. However differentiating between tumor types and determining their size can be difficult, which emphasizes the necessity for sophisticated diagnostic instruments (Ogunlade et al.).
Biomarkers as Indicators of Early Detection
Biomarkers play a crucial role in the early detection of astrocytomas, offering insights into tumor progression and patient prognosis. Finding particular molecular markers will aid in early tumor diagnosis, which is critical for better treatment results. Biomarkers such as MGMT promoter methylation and IDH1 mutations, for example, have been linked to improved survival rates and can direct individualized treatment plans (Margriet IJzerman-Korevaar et al.). Better patient outcomes ultimately result from early diagnosis by biomarkers, which not only allows for prompt intervention but also improves the precision of therapy approaches.
Machine Learning Algorithms in Early Diagnosis
Machine learning (ML) algorithms have been applied to improve early diagnosis and tumor progression prediction in recent studies. When it comes to creating diagnostic panels based on plasma metabolomics, machine learning methods like the Evolutionary Heterogeneous Decision Tree (EvoHDTree) have shown promise. These algorithms can examine sizable datasets to spot trends and more precisely forecast the existence of tumors (Godlewski et al.).
Advantages of Machine Learning in Predicting tumor Progression
When it comes to predicting the progression of tumors, machine learning provides various benefits, such as increased diagnostic accuracy and decreased misdiagnosis risk. Machine Learning (ML) can yield more accurate predictions regarding tumor behaviour and treatment response by utilizing sophisticated algorithms and integrating diverse data sources. This ability is especially helpful for managing astrocytomas, as prompt treatment can have a major effect on the prognosis of patients (Godlewski et al.).
Surgical Interventions
Craniotomy and tumor Resection
Astrocytomas are typically treated primarily with surgery. To reach and remove the tumor, a craniotomy requires part of the skull to be removed. The location of the tumor and the surrounding brain structures determine the extent of resection, which can range from partial to total (Kabel et al.). To lower the chance of a local recurrence, complete resection is desired; however, if the tumor is in a place that makes complete removal challenging, partial resection may be carried out (Ogunlade et al.).
Stereotactic Surgery
Using imaging techniques, stereotactic surgery locates the cancer precisely and guides surgical tools to it. This technique is especially helpful for tumors that are hard to reach during conventional surgery. According to Kabel et al., stereotactic biopsy or resection can be used to remove small, targeted cancer areas with little to no effect on the surrounding brain tissue or to get tumor samples.
Radiation Therapy
External Beam Radiation Therapy (EBRT)
Astrocytomas are often treated with external beam radiation therapy. It entails aiming externally directed high-energy X-rays at the cancer. After surgery, this technique is utilized to eradicate any cancer cells that remain, or it might be the principal treatment for tumors that are not treatable (Kabel et al.). When it comes to symptom management and tumor development control, EBRT can be useful.
Stereotactic Radiosurgery (SRS)
Extremely precise radiation therapy, known as stereotactic radiosurgery, targets the tumor with numerous focused radiation beams. It can be used to treat remaining cancer cells following surgery and is especially helpful for treating tiny or localized tumors (Willman et al.). Compared to conventional radiation therapy, SRS has fewer side effects and does less damage to the surrounding healthy tissue.
Proton Therapy
Proton therapy is a form of radiation therapy that treats cancer by using protons instead of X-rays. More accurate targeting of protons may limit injury to neighbouring healthy tissue. The efficacy of this approach in treating different kinds of astrocytomas is presently being investigated (Kabel et al.).
Chemotherapy
Standard Chemotherapeutic Agents (e.g., Temozolomide)
Drugs are used in chemotherapy to either kill or stop the growth of cancer cells. One popular chemotherapeutic drug for astrocytomas, particularly glioblastomas, is temozolomide. It inhibits the growth and multiplication of cancer cells by causing damage to their DNA (Willman et al.). Chemotherapy is effective, although its effect on overall survival may be limited, especially in high-grade tumors (Kabel et al.).
Targeted Drug Delivery Systems
The goal of targeted drug delivery systems is to spare healthy tissues while administering chemotherapeutic medications directly to cancer cells. This strategy can lessen negative effects and increase therapeutic efficacy. Developing drug delivery systems that employ nanoparticles or other techniques to enhance drug localization at the tumor site is one aspect of research into targeted therapies (Kessler et al.).
Immunotherapy
Immune Checkpoint Inhibitors
The purpose of immune checkpoint inhibitors is to strengthen the body's defences against cancerous cells. According to Kessler et al., these treatments focus on proteins that suppress immune system function, enhancing the immune system's capacity to identify and combat cancer cells. For astrocytomas, these treatments are still in the experimental stages, but they have the potential to enhance treatment results (Kessler et al.).
Vaccine-Based Therapies
The goal of vaccine-based treatments is to prime the immune system to identify and combat antigens unique to tumors. This approach includes developing vaccines targeting specific mutations or markers associated with astrocytomas, such as the IDH mutation (Kessler et al.). These vaccines may strengthen immune responses against brain tumors, according to preliminary experiments.
Emerging Therapies
Gene Therapy
The goal of gene therapy is to alter or rectify genetic alterations linked to cancer. This strategy involves introducing genetic material into tumor cells to either kill the cells directly or increase their susceptibility to other treatments for astrocytomas (Kessler et al.). There are still investigations being conducted to determine the safety and effectiveness of this field of study.
Anti-Angiogenic Therapy
Anti-angiogenic therapy stops cancer growth by focusing on the blood vessels that feed the tumors. Astrocytomas are among the malignancies that have been treated with agents that block vascular endothelial growth factor (VEGF) (Kessler et al.). The goal of these treatments is to slow the growth of the tumor and lessen tumor vascularization.
Personalized Medicine Approaches
Personalized medicine entails adjusting the course of treatment for the tumor's genetic makeup. To determine the best treatments for specific patients, this method makes use of proteomic and genetic data. Personalized treatments for astrocytomas might involve targeted therapies and customized chemotherapy regimens based on specific tumor mutations (Kessler et al.).
Integrative and Supportive Care
Palliative Care
Enhancing the quality of life for individuals with advanced or terminal cancer is the main goal of palliative care. It entails treating psychological and physical requirements, regulating symptoms, and offering emotional support (Ogunlade et al.). Enhancing the comfort and well-being of individuals with recurrent or incurable astrocytomas requires this kind of care.
Quality of Life Considerations
Examining how a patient's daily life is affected by their therapy is part of the quality of life considerations. This includes managing side effects, supporting cognitive and physical function, and providing resources for emotional and psychological support (Kessler et al.). Keeping patients' general well-being during treatment depends on these factors being effectively managed.
Complementary Therapies
In addition to traditional treatments, complementary therapies, including massage, acupuncture, and dietary modifications, are frequently employed to control symptoms and enhance general health. Although these therapies do not take the place of conventional medical care, they can improve patients' quality of life and provide extra support (Kessler et al.).
Conclusion
Summary of Current Treatment Landscape
Surgical approaches for treating astrocytomas include craniotomies and stereotactic surgery, which are designed to remove or sample tumors with the least amount of damage possible (Kabel et al.). While chemotherapy, most notably Temozolomide, is employed depending on cancer grade, radiation therapies, such as External Beam Radiation Therapy (EBRT) and Stereotactic Radiosurgery (SRS), accurately target tumors (Willman et al.). Along with immunotherapy and supportive care, emerging medicines, including gene therapy and anti-angiogenic therapy, offer new opportunities that improve patient management and quality of life (Kessler et al.).
The Role of Early Detection and Machine Learning
For astrocytomas, treatment outcomes are considerably improved by early identification. By evaluating intricate genetic and imaging data, machine learning improves diagnosis accuracy and becomes more accurate at predicting the course of tumors (Kessler et al.). These technological developments allow for earlier and more accurate interventions (Ogunlade et al.).
Statistics
Survival rate of Astrocytomas
Astrocytomas are a type of brain tumor for which the survival rate varies significantly depending on several factors, such as the tumor grade, location, size, age, and general health of the individual. However, astrocytomas account for more than 60% of all primary brain tumors. Although the survival rates reported by The Brain Tumor Research are estimates based on a large sample size, they may not accurately predict the outcome for a particular case. However, the surgical removal of the entire tumor is not feasible because there are almost 100% of the time remaining malignant tumor cells after a maximal surgical resection, they can only take out as much tumor as is safely possible with surgery.
The survival rates associated with different stages of astrocytomas:
Stage I Astrocytomas: The 5-year survival rate for grade I astrocytomas which is pilocytic astrocytomas is generally high, ranging from 90% to 100% because they are typically slow-growing and have a good chance of recovery from the disease.
Stage II Astrocytomas: The 5-year survival rate for grade II astrocytomas can range from 30% to 80%. This is a diffuse astrocytoma and has a variable prognosis, but these tumors still have the potential to transform into higher-grade tumors over time.
Stage III Astrocytomas: The 5-year survival rate for stage III astrocytomas, anaplastic astrocytomas, is typically lower, ranging from 20% to 45% and they are more severe than stage II Astrocytomas. Furthermore, these tumors possibly have a higher chance of recursion and development to a more critical stage because, in the brain, you cannot take the margin while in other areas of the body, they can resect normal tissue to make sure the entire tumor is removed.
Stage IV Astrocytomas: The 5-year survival rate for stage IV, glioblastomas, is genuinely low, ranging from 5% to 10%. It is the most life-threatening form of astrocytomas which are also associated with a poorer prognosis. Although there are a few poisonous treatments involved, the recursion rate is high and it is impossible to destroy the tumors completely.
Prognosis of Astrocytomas based on age
The 5-year relative survival rate for diffuse astrocytoma by age group is as follows:
Children (ages 0-14): 82.2%
Adolescents and Young Adults (ages 15-39): 77.6%
Adults (ages 40+): 33.1%
Table 1. The database shows the 5-year relative survival rate for diffuse astrocytoma by different age group
This piece of data that was obtained by the International Cancer Genome Consortium represents how the common age of diagnosis for astrocytoma ranges from ages 2-4. Exactly, 18 children out of 96, which is 18.75%, are diagnosed at the age of 2-4. After age 16, there is a sharp decline in what age develops Astrocytoma, indicating that this tumor grows especially in young children.
Table 2. Risk of developing second primary malignancy in malignant astrocytoma patients
Site of SPM | Observed | Expected | SIR | 95% CI |
Brain | 100 | 8.09 | 12.361 | 10.05–15.03 |
Cranial nerves other nervous system | 8 | 0.48 | 16.531 | 7.14–32.58 |
Endocrine system | 24 | 14.76 | 1.631 | 1.04–2.42 |
1P<0.05.
The overall risk of second primary malignancy among malignant astrocytomas was significantly higher than that in the general population (SIR: 1.09, 95% CI: 1–1.18, P<0.05). Specific sites where the risk increases include the brain, cranial nerves and other nervous systems when the tumors tend to undergo malignant changes and invade the surrounding brain tissues and the meninges.
Influence of latency, gender, and age upon diagnosis on the site-specific risk of SPM in patients with MA
Table 3. Effect of age at diagnosis and gender on the site-specific risk of SPM in MA patients.
Site of second malignancy | Age at diagnosis | Gender | |||
0–29 years SIR, 95% | 30–59 years SIR, 95% | ≥60 years SIR, 95% | Male SIR, 95% | Female SIR, 95% | |
Brain | 19.17 (12.01–29.02)1 | 17.47 (13.57–22.15)1 | 3.27 (1.57–6.02)1 | 10.58 (7.94–13.8)1 | 15.4 (11.27–20.54)1 |
Cranial nerves other nervous system | 27.91 (5.75–81.55)1 | 16.04 (4.37–41.07)1 | 7.87 (0.2–43.87) | 18.28 (5.94-42.67)1 | 14.26 (2.94–41.67)1 |
Endocrine system | 1.09 (0.13–3.95) | 2.06 (1.26–3.17)1,8 | 0.62 (0.08–2.26) | 2.67 (1.38–4.66)1,14 | 1.17 (0.6–2.04) |
Based on the age at malignant astrocytoma diagnosis, patients were divided into three different groups. The incidence of SPM rose considerably in individuals aged ≤29 and 30-59 years. Patients aged ≥60 showed a considerably lower probability of SPM. The overall risk of SPM in men and females did not alter when stratified by gender among MA patients.
Impacts
Introduction
Overview of Symptoms
Glioblastomas (GB) and other astrocytomas are a varied category of brain tumors that vary greatly in their symptoms according to the location and grade of the tumor. The frequency of symptoms such as headaches, seizures, and cognitive deficits emphasizes the extensive effects these tumors can have on patients' quality of life (Willman et al.). Astrocytomas are among the group of gliomas that frequently result in a variety of neurological, cognitive, and psychiatric symptoms that can have a major impact on day-to-day functioning and quality of life (Boele et al.). This result emphasizes how important it is to have thorough care plans and efficient symptom control.
Importance of Mental Health
Patients with astrocytomas should give careful thought to their mental health because the condition and its treatment can cause severe emotional and psychological anguish. Mood disorders, behavioural changes, and personality changes are frequent and can increase the disease's overall burden (Boele et al.). Improving the general health and quality of life of patients receiving therapy for astrocytomas requires addressing these factors (Margriet IJzerman-Korevaar et al.).
Neurological Symptoms
Headaches
Patients with astrocytomas frequently experience headaches, which are frequently caused by elevated intracranial pressure or brain abnormalities connected to the tumor (Ogunlade et al.). The size, location, and grade of the tumor can all have a major impact on the frequency and severity of headaches. Chronic headaches that do not go away with traditional pain relief techniques could be a sign of a tumor's advancement or a need for additional care (Kessler et al.).
Seizures
Another typical sign of astrocytomas is seizures, especially when the tumors are situated in areas of the brain that regulate movement and sensory perception (Willman et al.). Seizures are common in glioma patients; over 37% of patients report having this symptom (Margriet IJzerman-Korevaar et al.). Since the nature and intensity of seizures might differ, specialized treatment methods are needed to successfully manage and control them (Boele et al.).
Cognitive and Physical Impairments
Memory Issues
Patients suffering from astrocytomas frequently experience cognitive deficits, such as memory problems. These problems are frequently brought on by tumor involvement in the brain regions in charge of memory and executive function (Boele et al.). Early assessment and intervention are essential for effectively treating symptoms of cognitive impairments since they can have an influence on daily activities and overall quality of life (Margriet IJzerman-Korevaar et al.).
Coordination Problems
Patients with astrocytomas frequently experience coordination issues, including issues with balance and motor abilities, especially when the tumor impacts the brain's motor regions (Ogunlade et al.). These disabilities can make it difficult to carry out daily duties and preserve independence, which emphasizes the need for focused therapy and rehabilitation (Kessler et al.).
Management Strategies
Medical Interventions
Radiation therapy, chemotherapy, and surgical excision are among the medical methods used to treat astrocytoma symptoms. As much of the tumor as possible is removed during a surgical resection, which can reduce symptoms and enhance results (Kabel et al.). To target remaining cancer cells and stop recurrence, chemotherapy and radiation therapy are frequently employed in conjunction with surgery (Willman et al.). Treatment approaches, such as immunotherapies and targeted treatments, are always being improved to increase effectiveness and reduce adverse effects (Kessler et al.).
Supportive Therapies
Managing the psychological and emotional effects of having an astrocytoma is greatly aided by supportive therapy. Psychotherapy therapies including cognitive-behavioral therapy (CBT) can assist treat mood disorders and enhance coping skills (Boele et al.). Furthermore, to address cognitive and physical deficits and improve overall quality of life, supportive care services—such as neuropsychological tests and rehabilitation—are crucial (Margriet IJzerman-Korevaar et al.).
Mental Health Impacts
Psychological Effects
Anxiety and depression are two major psychological symptoms that patients with astrocytomas frequently face. Elevated levels of anxiety and depression symptoms might result from the stress of receiving a cancer diagnosis, as well as the difficulties associated with therapy and symptom management (Boele et al.). Uncertainty regarding the prognosis and course of therapy might cause anxiety, but the emotional toll that the illness has on daily life can lead to depression (Margriet IJzerman-Korevaar et al.). It is imperative to address these psychological consequences to promote better outcomes in terms of mental and physical health as well as overall well-being.
Social Isolation
Significant social isolation may result from the way astrocytomas affect social interactions. Due to physical restrictions, mental problems, or emotional anguish, patients may stop participating in social activities, which can worsen depressive and lonely feelings (Boele et al.). Maintaining social ties is crucial for patients' mental health, and social support has a significant role in overall quality of life (Margriet IJzerman-Korevaar et al.).
Daily Activity Changes
The repercussions of astrocytomas, such as physical limitations and cognitive difficulties, frequently disturb daily activities and routines (Kessler et al.). A patient's sense of control and quality of life may be negatively impacted by changes in their capacity to carry out daily duties, which may result in less independence and a greater need for caregivers (Ogunlade et al.). Patients' capacity to participate in everyday activities can be improved and these interruptions can be lessened with the use of supportive therapies and methods.
Support and Coping
Counselling and Support Groups
For patients with astrocytomas, counselling and support group participation can be very beneficial. These tools can reduce feelings of loneliness and aid in the management of psychological discomfort because they provide coping mechanisms, emotional support, and a sense of community (Boele et al.). Patients with brain tumors might benefit greatly from peer support and useful guidance in overcoming the obstacles of their condition from support groups designed especially for them (Margriet IJzerman-Korevaar et al.).
Stress Management Techniques
Patients with astrocytomas must learn effective stress management strategies. Stress can be decreased and emotional well-being can be enhanced by methods including mindfulness, relaxation techniques, and cognitive-behavioural therapies (Kessler et al.). Better coping strategies and an overall higher quality of life can be supported by incorporating these tactics into everyday routines (Boele et al.).
Summary
Patient Impacts
Patients with astrocytomas experience severe effects on their neurological and cognitive capacities as well as their general quality of life. The wide spectrum of symptoms, which include headaches, seizures, memory loss, and coordination problems, highlights how difficult it is to manage this illness. Anxiety, despair, and social isolation are examples of mental health issues that exacerbate the patient's condition. Addressing the complex effects of astrocytomas requires comprehensive care techniques that include medical interventions, supportive therapies, and psychological support.
Importance of Integrated Care
To effectively address the different requirements of patients with astrocytomas, an integrated care approach is essential. Together with medical care, social services, psychological support, and rehabilitation can improve general health and quality of life. Healthcare professionals may give patients a more comprehensive and encouraging care experience by addressing the effects of astrocytomas on both physical and mental health, which will eventually improve patients' well-being and treatment success.
Conclusion
All in all, astrocytoma is a type of brain and spinal cord tumor that originates from Gliomas (glial cell tumors). Astrocytoma is proven to be more prevalent in children compared to adults. Future studies have to be conducted as to why cell growth is higher in children compared to adults. Some symptoms of astrocytoma include headache & seizures, imbalance and coordination issues, speech difficulties, weakness, nausea & vomiting, and cognitive/behavioural changes. Additionally, some equipment used to accurately diagnose astrocytoma consists of conventional MRIs, contrast-enhanced MRIs, perfusion MRIs, diffusion-weighted MRIs, computer tomography scanners, positron emission tomography scanners, biopsy, electroencephalography, angiography, intraoperative monitoring equipment, and neurophysiological testing. There are also many medical professions to assist in helping patients such as neurosurgeons, neurologists, neuro-oncologists, radiation oncologists, and many more. Many treatments have also been researched to reduce the risk and growth of astrocytoma; some of these include biomarkers (help detect astrocytoma early on), machine learning algorithms including Evolutionary Heterogeneous Decision Trees (can observe datasets to notice trends and predict the location of the tumor). Additionally, many surgeries are aimed towards removing astrocytoma such as craniotomy tumor resection and stereotactic surgery. Other treatments consist of therapeutic ways to approach the tumor which are chemotherapy, immunotherapy, and some emerging therapies for example gene therapy. Dietary modification and enhancing the quality of life are equally important when it comes to controlling the growth of the tumor. Astrocytoma can be divided into different grades where there are different rates of survival. One correlation noticed includes how when the age increases, survival rates decrease. Finally, astrocytoma can take a toll on mental health and cause cognitive & physical impairments. Some suggestions to manage the effects of astrocytoma include medical interventions, supportive therapies, support groups, stress management techniques, and most importantly, being able to manage a rich quality of life.
Machine Learning
Machine Learning has an integral part in astrocytoma. Machine learning algorithms have been shown to improve early diagnosis and tumor progression prediction in recent studies. Machine learning can help in various ways including increased diagnostic accuracy and decreased misdiagnosis risk.
Future Implications
Since astrocytoma is very common in children, it is important to bring awareness to this tumor. Some ways to do this include, creating educational campaigns, advocating for funding of research on tumors, creating educational programs in schools to talk about brain health, and holding awareness events. Future research must focus on how to reduce the growth of astrocytoma in children and potential treatments. Studies should also focus on research about the growth of astrocytoma compared between children and adults and why growth doesn’t occur in other organs.
Bibliography (MLA 9th Gen)
1. Kabel, Ahmed M., et al. “Astrocytoma: Insights into Risk Factors, Pathogenesis, Diagnosis and Management.” Journal of Cancer Research and Treatment, vol. 6, no. 3, Aug. 2018, pp. 70–73, https://doi.org/10.12691/jcrt-6-3-2. Accessed 8 Aug. 2024.
2. Ogunlade, John, et al. “Primary Spinal Astrocytomas: A Literature Review.” Cureus, Cureus, Inc., July 2019, https://doi.org/10.7759/cureus.5247. Accessed 8 Aug. 2024.
3. Willman, Matthew, et al. “Update for Astrocytomas: Medical and Surgical Management Considerations.” PubMed Central, National Institutes of Health, Feb. 2023, pp. 1–26, https://doi.org/10.37349/en.2023.00009. Accessed 8 Aug. 2024.
4. Godlewski, Adrian, et al. “A Comparison of Different Machine-Learning Techniques for the Selection of a Panel of Metabolites Allowing Early Detection of Brain Tumors.” Scientific Reports, vol. 13, no. 1, Nature Portfolio, July 2023, https://doi.org/10.1038/s41598-023-38243-1. Accessed 8 Aug. 2024.
5. Kessler, Tobias, et al. “Conventional and Emerging Treatments of Astrocytomas and Oligodendrogliomas.” Journal of Neuro-Oncology, vol. 162, no. 3, Springer Science+Business Media, Dec. 2022, pp. 471–78, https://doi.org/10.1007/s11060-022-04216-z. Accessed 8 Aug. 2024.
6. Margriet IJzerman-Korevaar, et al. “Prevalence of Symptoms in Glioma Patients throughout the Disease Trajectory: A Systematic Review.” Journal of Neuro-Oncology, vol. 140, no. 3, Springer Science+Business Media, Oct. 2018, pp. 485–96, https://doi.org/10.1007/s11060-018-03015-9. Accessed 8 Aug. 2024.
7. Boele, Florien W., et al. “Psychiatric Symptoms in Glioma Patients: From Diagnosis to Management.” Neuropsychiatric Disease and Treatment, Dove Medical Press, June 2015, pp. 1413–13, https://doi.org/10.2147/ndt.s65874. Accessed 8 Aug. 2024.
8. Research, Brain Tumour. “What is the survival rate of astrocytoma?” Brain Tumour Research, 23 Oct. 2023. Accessed 10th Aug, 2024. https://braintumourresearch.org/blogs/faq/what-is-the-survival-rate-of-astrocytoma#:~:text=The%205%2Dyear%20survival%20rate,from%2030%25%20to%2080%25.
9. CBTRUS (2008) CBTRUS Statistical Report. Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2004-2008, Central Brain Tumor Registry of the United States, 2000-2004.
10. “Doctors Who Treat Astrocytomas | Neurological Surgery.” Weillcornell.org, Weill Cornell Medicine, 2024, neurosurgery.weillcornell.org/condition/astrocytoma/doctors-who-treat-astrocytomas#:~:text=A%20patient%20diagnosed%20with%20an. Accessed 10 Aug. 2024.
11. “International Neurologist Salary.” ZipRecruiter, 3 Aug. 2024, www.ziprecruiter.com/Salaries/International-Neurologist-Salary#:~:text=International%20Neurologist%20Salary&text=%24320%2C500%20is%20the%2025th%20percentile,Salaries%20below%20this%20are%20outliers.&text=%24400%2C000%20is%20the%2090th%20percentile. Accessed 10 Aug. 2024.
12. Mendoza, Alejandro Arias, et al. “Astrocytoma, Diagnosis and Treatment. Literature Review.” International Journal of Medical Science and Clinical Research Studies, vol. 03, no. 01, Jan. 2023, https://doi.org/10.47191/ijmscrs/v3-i1-04. Accessed 16 Feb. 2023.
13. Nabity, Justin. “Neurosurgeon Salary: What Should You Earn?” Physicians Thrive, 11 Dec. 2021, physiciansthrive.com/physician-compensation/neurosurgeon/.
14. “The Average Radiation Oncology Salary [+ Interesting Insights].” Physicians Thrive, Physicians Thrive, 6 June 2024, physiciansthrive.com/physician-compensation/radiation-oncology-salary/#:~:text=The%20average%20radiation%20oncologist. Accessed 10 Aug. 2024.
15. “Neuro-Oncology Physician Salary.” ZipRecruiter, 5 Aug. 2024, www.ziprecruiter.com/Salaries/Neuro-Oncology-Physician-Salary. Accessed 12 Aug. 2024.
16. “Radiation Therapy for Glioma & Astrocytoma.” Nyulangone.org, 2024, nyulangone.org/conditions/glioma-astrocytoma/treatments/radiation-therapy-for-glioma-astrocytoma#:~:text=Doctors%20use%20external%20beam%20radiation. Accessed 10 Aug. 2024.
17. “What Is a Neurosurgeon - Neurosurgery - Highland Hospital - University of Rochester Medical Center.” Www.urmc.rochester.edu, www.urmc.rochester.edu/highland/departments-centers/neurosurgery/what-is-a-neurosurgeon.aspx#:~:text=Four%20years%20of%20medical%20school.
18. “Patient Care at NYU Langone Health.” Nyulangone.org, 2024, nyulangone.org/. Accessed 11 Aug. 2024.
19. “Astrocytoma | Neurological Surgery.” Weillcornell.org, Weill Cornell Medicine, 2022, neurosurgery.weillcornell.org/astrocytoma. Accessed 11 Aug. 2024.
20. “Atelectasis - Symptoms and Causes.” Mayo Clinic, 2023, www.mayoclinic.org/diseases-conditions/atelectasis/symptoms-causes/syc-20369684. Accessed 11 Aug. 2024.
21. “MD Anderson Cancer Center.” MD Anderson Cancer Center, 2024, www.mdanderson.org/. Accessed 11 Aug. 2024.
22. Wachtel, Andrew. “Barrow Neurological Institute.” Barrow Neurological Institute, 30 July 2024, www.barrowneuro.org/. Accessed 11 Aug. 2024.
23. “Astrocytoma | Brain Tumour Types.” Brain Tumour Research, 2024, braintumourresearch.org/en-ca/pages/types-of-brain-tumours-astrocytoma. Accessed 11 Aug. 2024.
24. Pichaivel, Manimekalai, et al. ‘An Overview of Brain Tumor’. Brain Tumors, IntechOpen, 20 Apr. 2022. Crossref, doi:10.5772/intechopen.100806. Accessed 10 Aug. 2024.
25. “Brain and Spinal Cord Tumors” National Institute of Neurological Disorders and Strokes https://www.ninds.nih.gov/health-information/disorders/brain-and-spinal-cord-tumors. Accessed 9 Aug. 2024.
Cervicomedullary astrocytomas of childhood: clinical and imaging follow-up. T Young Poussant, N Yousouf, P D Barnes, D C Anthony, D Zurakowski, R M Scott, N J Tarbell. https://pubmed.ncbi.nlm.nih.gov/10460326/
Development of anaplastic changes in low-grade astrocytomas of childhood. Dirks PB, Jay V, Becker LE, Drake JM, Humphreys RP, Hoffman HJ, Rutka JT. https://pubmed.ncbi.nlm.nih.gov/8121571/#:~:text=Development%20of%20anaplastic%20changes%20in%20low%2Dgrade%20astrocytomas%20of%20childhood
Clinical Features, Treatment and Outcome of Childhood Glial Tumors. Kara B, Ertan K, Karabagli H, Yavas G, Caglayan AO, Koksal Y. https://pubmed.ncbi.nlm.nih.gov/34751424/
Management of Holocord pilocytic astrocytomas in children and adolescents: an update. Ebner FH, Schittenhelm j,Roser F, Scheel-Walter H, Tatagiba M, Schuhmann MU. https://www.google.com/url?sa=t&source=web&rct=j&opi=89978449&url=https://pubmed.ncbi.nlm.nih.gov/23429240/&ved=2ahUKEwj21Pb39-6HAxUyW0EAHSMJCH4QFnoECBMQAQ&usg=AOvVaw17EO23zhVjBphnD50zUkQm
Surgical treatments of patients with low-grade astrocytomas and medically intractable seizures. Gunnarsson T, Olafsson E, Sighvatsson V, Hannesson B. https://www.google.com/url?sa=t&source=web&rct=j&opi=89978449&url=https://pubmed.ncbi.nlm.nih.gov/11939941/&ved=2ahUKEwjN2syG-O6HAxVZW0EAHWDHKw4QFnoECBgQAQ&usg=AOvVaw1D-7BBBKIahKzowCBYLJhE
Imaging characteristics and growth of subependymal giant cell astrocytomas. Clarke MJ, Foy AB, Wetjen N, Raffel C. https://www.google.com/url?sa=t&source=web&rct=j&opi=89978449&url=https://pubmed.ncbi.nlm.nih.gov/16459995/&ved=2ahUKEwjq1_Ob-O6HAxW9T0EAHal6Ov8QFnoECBsQAQ&usg=AOvVaw2VUjwcBjIQjQ08TubrxqzR
Role of Intraoperative Neurophysiologic Monitoring In the Resection Of Thalamic Astrocytomas. Carraba G, Bertani G, Cogiamanian F, Ardolino G, Zarino B, Di Cristofori A, Locatelli M, Caroli M, Rampini P. https://www.google.com/url?sa=t&source=web&rct=j&opi=89978449&url=https://pubmed.ncbi.nlm.nih.gov/27338215/&ved=2ahUKEwjgq8K0-O6HAxX2R0EAHcmLFawQFnoECBcQAQ&usg=AOvVaw2gnJgIKO7I4ABdEbw-QPOA
Seizures in patients with IDH-mutated lower grade gliomas. Carstam L, Ryden I, Jakola AS. https://www.google.com/url?sa=t&source=web&rct=j&opi=89978449&url=https://pubmed.ncbi.nlm.nih.gov/36258151/&ved=2ahUKEwjYtpbJ-O6HAxV-VEEAHfD9O1YQFnoECA8QAQ&usg=AOvVaw3dSbwNXKM2j8Sd-0Bgf7EK
Astrocytoma Brain Imaging: Practice Essentials, Computer Tomography, Djamil Fertikh, L. Gill Naul. https://www.google.com/url?sa=t&source=web&rct=j&opi=89978449&url=https://emedicine.medscape.com/article/336695-overview&ved=2ahUKEwiT1ZuU-e6HAxVzSUEAHcm6KqkQFnoECBkQAQ&usg=AOvVaw1NNbQ6AeRY8G4lOpswdeyl
Astrocytoma, IDH-mutant, Radiology Reference. Rohit Sharma. https://www.google.com/url?sa=t&source=web&rct=j&opi=89978449&url=https://radiopaedia.org/articles/astrocytoma-idh-mutant-1&ved=2ahUKEwiT1ZuU-e6HAxVzSUEAHcm6KqkQFnoECDAQAQ&usg=AOvVaw2S2e6NBI_-alC13M4qxKt4
Indocyanine green angiography of retinal astrocytomas associated with tuberous sclerosis. Nilufer Koak. https://www.google.com/url?sa=t&source=web&rct=j&opi=89978449&url=https://pubmed.ncbi.nlm.nih.gov/14717494/&ved=2ahUKEwjkw7zqke-HAxWFWEEAHWYTCuwQFnoECBkQAQ&usg=AOvVaw26IYafwu4GoBjFxl1yvBKW
Astrocytomas: Symptoms, Causes and Treatment. Kenneth D. Aldape. https://www.google.com/url?sa=t&source=web&rct=j&opi=89978449&url=https://rarediseases.org/rare-diseases/astrocytoma/&ved=2ahUKEwjrxrGGk--HAxV-VUEAHZhKMqIQFnoECDUQAQ&usg=AOvVaw3z83EEpEu3YmcF4erd5Wpv
Cognitive, language, and school performance in children and young adults treated for low‐grade astrocytoma in the posterior fossa in childhood. Ingela Kristiansen, Cristina Eklund, Margareta Strinnholm, Bo Strömberg, Maria Törnhage, Per Frisk. https://www.google.com/url?sa=t&source=web&rct=j&opi=89978449&url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8955056/&ved=2ahUKEwiw7M_rk--HAxVjZ0EAHUVNBZ0QFnoECBIQAQ&usg=AOvVaw08ckMQNM1YBV3A2RCytJNZ
Acknowledgements
We acknowledge GenWriters and Sunshine 4 Cancer Kids for consulting and running lessons on the topics discussed in the paper. We acknowledge SlidesGo as the template on which the presentation of this paper is based.
Role of the Funding Source
No Funding was received or used.
Declaration of Interest
None.





Comments